Physics Research
The Physics Research Group is led by Professor Alan Nahum. Our principal research interests concern radiobiological modelling for the evaluation and optimisation of radiotherapy. Specific projects include the following:
- Modification of the Pinnacle Research Interface (PRI) to enable biologically optimised “inverse planning” of intensity-modulated treatments; e.g. maximising tumour (local) control (TCP) at a fixed complication risk (NTCP).
- Creation of a phase-II (3-arm) trial protocol for prostate radiotherapy, BioProp, including the use of functional MR images of clonogen concentration for radiobiologically guided dose painting.
- Designing three phase I/II trials of dose-escalated, accelerated radiotherapy for non-small cell lung cancer (NSCLC), in collaboration with clinicians in London, Cardiff, Glasgow and Sheffield. We have also developed advanced quality assurance methodologies for these trials, which depend on accurate dose calculations in lung tissue.
- Developing software for the radiobiological optimisation of treatment planning. BioSuite enables “isotoxic” (iso-NTCP) customisation of both the prescription dose and the number of fractions, taking account of tumour proliferation, given the tumour and normal-tissue DVHs.
- Development of a delay-differential model of the variation of stem-cell number with time during radiation treatments, which we are using to study the effects of schedule adaptation and individualisation strategies. The model links compensatory proliferation kinetics in early-reacting tissues to the degree of tissue damage, and addresses radiation and chemo-radiation schedule effects that are not analysable using simpler approaches. Figure 1
- A sequential PET fluorothymidine imaging study for NSCLC and head-and-neck squamous-cell carcinoma patients, in collaboration with colleagues at St. Thomas’ Hospital, London. This study aims to characterise the spatio-temporal stability of tumour proliferation patterns, which impacts on both the potential for selectively boosting hyperproliferative tumour regions, and on dynamic schedule. We are also developing multi-scale models of epithelia where early radiotherapy reactions arise, again exploring the potential of dynamically modified radiotherapy schedules.
- Use of the “dose accumulator” of the PRI together with 4DCT images to examine the effects of lung tumour motion (e.g., due to respiration) on conformal dose distributions, including the novel strategy of a deliberate reduction of field sizes under an isotoxic constraint (in collaboration with Tony Popescu, Vancouver).
- Monte-Carlo modelling of the Clatterbridge proton beamline, predicting dose distributions for arbitrary modulation of passively-scattered beams. This involves investigating the effects of beam modifiers and comparing them with film and polymer gel measurements. Figure 2
- Applying Monte-Carlo techniques to characterise the dosimetry of small radiation fields, as used in IMRT and stereotactic radiosurgery, and exploring the implications of different detector designs. Figure 3
- Investigation of a device which detects the change in air temperature between inhalation and exhalation, and its application to respiratory-gated treatment (a former PhD project).
- Pareto-optimisation methodologies for arc-based IMRT planning, in order to develop a system that can rapidly generate IMRT plans. This would allow clinicians to explore several plans interactively, to see which offers the best trade-off between the multiple objectives. Figure 4
- Implementation of Monte-Carlo-based dose computation for the QA of treatment plans (including RapidArc rotational IMRT) in collaboration with Tony Popescu (Vancouver), Emiliano Spezi (Cardiff) and the Computing Department of the University of Liverpool.
- Conventional ideas on the radiobiology of fractionation have been re-examined and found to be inadequate when considering “parallel” organs, such as (normal) lung tissue. New theoretical insights have been gained, which demonstrate that much larger fraction sizes can be used for cases where organs at risk respond in a parallel fashion (in collaboration with Aswin Hoffmann, Nijmegen).
- A radiobiologically based, mechanistic computer simulation of the response of normal tissues to irradiation has been constructed. Through “virtual irradiation” of the voxelised organ, this is yielding valuable insights into the validity of several much simpler, analytical models of complication probability that are in common use.
Current PhD projects:
- Using radiobiological modelling to quantify the effect on clinical outcomes caused by the dosimetric uncertainties in commercial treatment planning systems, (due to their use of approximate algorithms), compared to experimentally-verified Monte Carlo as the “gold standard”.
- Building a computer model of a moving tumour, to investigate the relationship between movements, margin size and tumour local control as a function of the radiobiological parameters in the TCP model.
- Exploring dosimetric and radiobiological aspects of rotational IMRT.
- Comparing breath-hold, respiratory-gated and free-breathing radiotherapy techniques for lung cancer and deriving optimal treatment margins from 4DCT data via deformable registration.
We have external collaborations with John Fenwick (Oxford), Mauro Lori (Reggio Emilia), Tony Popescu (Vancouver), Vanessa Panettieri (Melbourne) and Aswin Hoffmann (Nijmegen).
You can access our recent physics research output here.
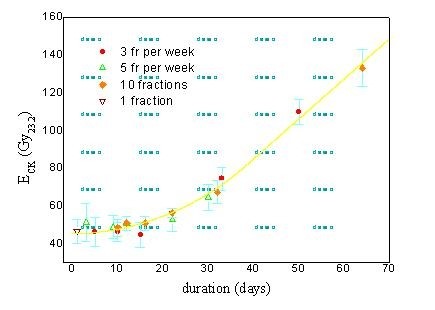
Figure 1. Fit of a delay-differential model to data on early radiotherapy reactions.
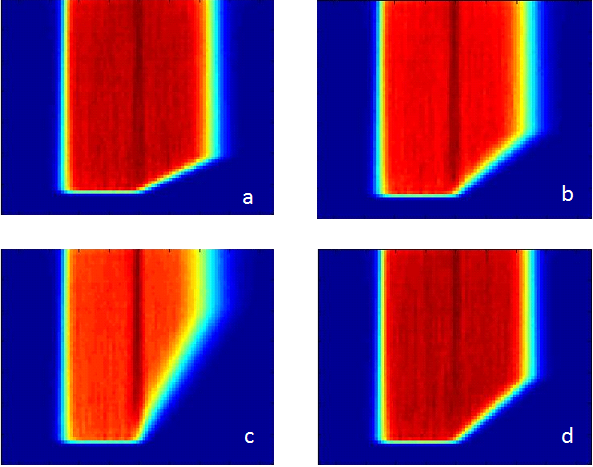
Monte-Carlo simulated proton dose in water beneath aluminium wedges of angles (in Al) of (a) 13.1°, (b) 22.8° and (c) 40.9°, and (d) for a PMMA wedge equivalent to the 22.8° Al wedge. Colourwash is normalised to the maximum dose, illustrating reduced in-
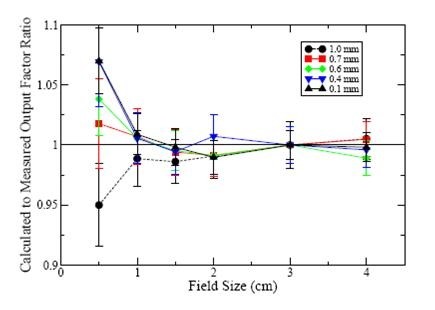
Impact of the width of the “raw” electron pencil beam on (Monte-Carlo modelled) radiation dose at the centre of small fields.
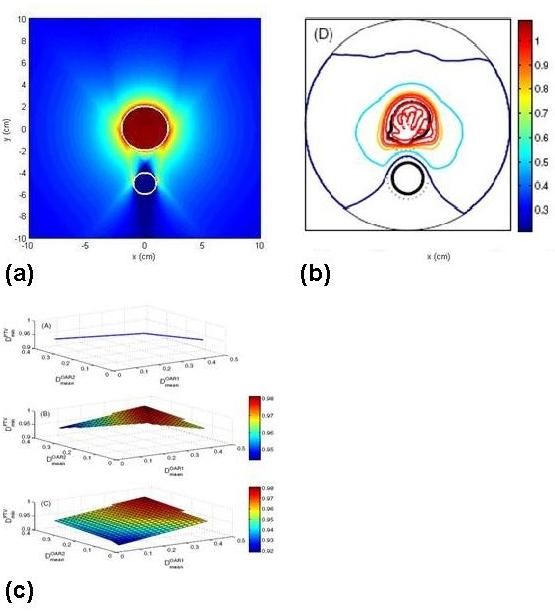
Figure 4. Pareto-optimisation approaches: (a), (b) analytically- and iteratively-derived homogenised arc dose distributions; (c) trade-off surfaces between different plans.
